INTRODUCTION
Anorectal melanoma (ARM) is an extremely rare and highly aggressive malignant lesion. It presents a low incidence, comprising between 0.05% and 4.6% (depending on the geographical area)1. Most ARM patients are caucasian females, aged 60–90 years. The most common symptoms described include abdominal pain, anal bleeding and constipation1. Non-specific symptoms can lead to a difficult differential diagnosis, since 25% of the ARMs have an amelanotic histological appearance (lack of pigmentation) and can be easily misdiagnosed as a benign polyp, adenocarcinoma, or clinically as hemorrhoids2.
The current available data are inconclusive and do not allow the formulation of guidelines regarding the optimal treatment strategy. Although no therapeutic consensus exists, wide local excision (LE) and abdomino-perineal resection (APR) are considered as the main therapies, with no difference in survival rates3-5. If technically feasible, wide local excision may represent a less invasive surgical procedure, maintaining the anal sphincter and patient’s quality of life4,5.
CASE PRESENTATION
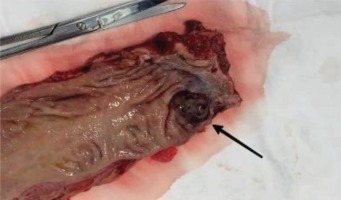
A patient aged 65 years in a good general condition was presented complaining of a specific clinical symptomatology, with episodic perineal pain, discomfort and rectal bleeding. A rectoscopy was carried out revealing an anal canal tumor mass that was biopsied. After a detailed dermatological examination, no other skin lesions were found, suggesting that the anorectal localization was the only primary site of the tumor. The pathological examination revealed a proliferation with granulation tissue, overlying fibrinematic and neutrophilicexudate, solid pattern consisting of large epithelioid cells with eosinophilic cytoplasm, intracytoplasmic granular brown pigment deposits, vesicle nuclei with eosinophilic macronucleoli and frequent atypical mitosis, an aspect compatible with the diagnosis of ulcerated malignant melanoma (Figure 1).
Figure 1
Hematoxylin-eosin staining of colonic tissue biopsy showing: a) epithelioid cells with eosinophilic cytoplasm, intracytoplasmic granular brown pigment deposits, vesicle nuclei with eosinophilic macronucleoli (OB 10X), and b) granulation tissue, overlying fibrinematic and neutrophilicexudate (OB 20X)
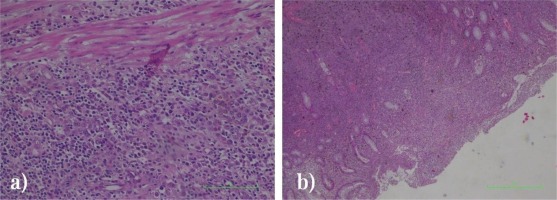
The analysis of haematological and biochemistry analytes indicated a normochromic normocytic anemia. There were no signs of locoregional or presence of distant metastasis on the performed staging workup, including staging MRI and CT scans. The MRI of the pelvis detected a circumferential parietal thickening of approximately 19 mm, posteriorly accentuated at the level of the anal canal about 4.4 cm long, at 2 cm from the external anal orifice, causing the subtotal obstruction, with no serosa or levator muscles’ infiltration (Figure 2).
Figure 2
Pelvic MRI: a) transversal view, arrow indicating anal tumor partially stenotic, and b) frontal view, cranio-caudal grown anal tumor
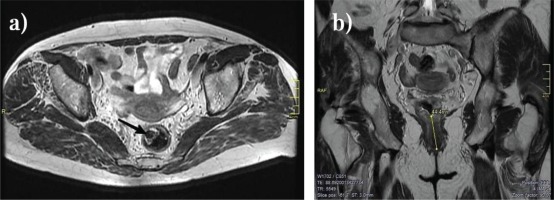
The patient underwent an APR with an R0-resection (Figure 3). Consequently, the postoperative course was favorable with fast recovery and no complications. The patient regained normal bowel movements on the 13th postoperative day. Two years later, no complications occurred and the patient is still followed up regularly (every 6 months, with imaging, hematological and biochemical tests), with no signs of local or distant tumor recurrence.
DISCUSSION
ARM therapeutic management strategies have not been well established, due to the lack of available randomized control trials. The treatment of ARM is mainly surgical, but the optimal approach is still debatable. The principal surgical procedure can be either APR or LE.
Brady et al.6 reviewed retrospectively a total of 85 cases and found that the overall survival for these patients was very poor (17% at 5 years; median, 19 months). The authors showed that APR can be considered as the preferred surgical approach for localized ARM. Long-term survival was better in the APR group versus local surgical procedures (27% vs 5%; p=0.11).
The invasion of the submucosa allows tumor cells to gain access to lymphovascular pathways, accelerating tumor growth. As a result, the depth of the tumor invasion determines the chances of lymphatic dissemination, rather than the thickness of the lesion, similar to the behavior of adenocarcinomas7. The presence of lymph node involvement is a negative prognostic factor and it is associated with a high mortality rate, especially in case of mesenteric lymphadenopathy. Perez et al.8 found a higher disease-specific survival in cases with clinically negative inguinal lymph nodes. The investigators concluded that lymphadenectomy should be reserved only for gross symptomatic disease. Another negative powerful prognostic factor is the presence of tumor perineural invasion (PNI). Perez et al.8 indicated that PNI was significantly correlated with recurrence-free survival because in their study all PNI patients experienced recurrence 2 years after surgery (p=0.002).
The surgical treatment decision (LE vs APR) should be individualized9,10. Temperley et al.9 performed a meta-analysis that included 10 studies and 303 patients. The main aim of the review was to compare LE and APR outcomes. The review included a total of 303 patients. The authors observed that despite the slightly better 5-year survival rate of LE (32% vs 23%), a statistically significant reduction in recurrence was found in APR group (OR=0.15; 95% CI: 0.08–0.28, p<0.00001)9. Lei et al.11 analyzed 795 ARM patients from the USA Surveillance, Epidemiology, and End Results (SEER) database. A nomogram based on a multivariate Cox regression model was generated to predict ARM-Specific Survival. The nomogramC-index was 0.74 (95% CI: 0.71–0.77) on internal verification, and in the validation cohort the nomogram C-index was 0.72 (95% CI: 0.68–0.76). The propensity score matching analysis results showed that patients who underwent surgery achieved a statistically significant overall survival (log-rank=17.41, p<0.001; ARM-Specific Survival: log-rank=14.55, p<0.001). Patients were stratified into LE and extended surgery (ES) groups, but the results were not statistically significantly different between the two subgroups (all p>0.05) and ES may not improve ARM-Specific or Overall Survival11. A recent systematic review and meta-analysis by Jutten et al.12-14 identified 347 studies and included 34 studies, with a total of 1858 ARM patients. They found that, regardless of stage, no significant difference in overall survival was found between the two surgical approaches (LE or ER). The authors found: in stage I, odds ratio 1.30 (95% CI: 0.62–2.72, p=0.49); in stage II, odds ratio 1.61 (95% CI: 0.62–4.18, p=0.33); and in stages I-III, odds ratio 1.19 (95% CI: 0.83–1.70, p=0.35)12-14.
Surgery is beneficial in cases without evidence of metastatic disease. In case of stage IV, a survival benefit was found because of immunotherapy and targeted therapies15. Treatments that inhibit the activity of type III transmembrane receptor tyrosine kinase KIT have been investigated by using imatinibmesylate and very good clinical responses were obtained, but only in the case of malignancies with demonstrated functional KIT mutations as demonstrated by Kim et al.15 and Carvajal et al.16. The study led by Taylor et al.17 affirms that the 2-year survival of ARM patients treated with immunotherapy increased, without any influence of their survival at 5 years though. Thus the research of new molecules is encouraged to change the treatment from a palliative to a curative one.
The most appropriate treatment strategy for ARM remains controversial regarding both the use and timing of radiotherapy (RT) in neoadjuvant or adjuvant setting. Patients who underwent LE with adjuvant chemotherapy and/or RT had a similar cancer-specific survival compared to those who underwent only ES18. In two single center studies, Ballo et al.19 and Kelly et al.20 evaluated 23 and 54 patients, respectively, who underwent LE, nodal dissection, and adjuvant RT and both have shown that the regimen has adequate local-regional disease control and is well tolerated. Ballo et al.19 reported a 5-year local and regional nodal control with rates of 74% and 84%, respectively, and Kelly et al.20 achieved a 5-year local control rate of 82%. Neo-adjuvant chemo-irradiation (CRT) was performed in order to achieve a pathological response, a negative margins excision and render a sphincter preservation feasible21,22.
CONCLUSION
ARM is an exceptionally rare disease with poor survival. Although the optimal therapeutic approach has not yet been established, surgery remains the only effective therapy23,24. The role of RT is still controversial, while new immunotherapeutic treatments are being developed. The main prognostic factors are tumor extent/stage, presence of perineural invasion and/or lymphnodal metastasis. LE is sufficient when free resection margins may be achieved, because ARM disseminates along the submucosal planes. In case of larger tumors or sphincter infiltration, an APR is required with curative intent25. Regional lymphadenectomy is advised when regional lymph node metastases are present. Palliative surgery may be warranted in case of distant metastases presence (metastasectomy) and in cases of refractory pain or incontinence.