The last 10 years, despite global scientific and technological progress, there has been an outbreak of chronic diseases, viral epidemics and pandemics, with a significant number of deaths, depletion of health systems and rising healthcare costs, leading to devastating economic, political and social consequences. Here, we describe briefly the human defence system, how environmental factors and mechanisms interfere with it, and the correlation with chronic exposure to environmentally toxic mixtures. Also, we examine the technologies that can increase viral aggression, focusing on the recent COVID-19 pandemic of the SARS-CoV-2 virus.
Immune system and immunity
The immune system is a defence network of immune cells and organs that work together to defend the human body. The immune response to xenobiotics includes the humoral immune response of T helper lymphocytes that produce cytokines to neutralize xenobiotics before they enter the cells and the cellular immune response to primary and adjuvant immune cells. In the cellular immune response are activated special subgroups of T-lymphocytes called CD4+ T-lymphocytes (that indirectly destroy cells identified as foreign and threatening), CD8+ T-lymphocytes or killer T cells (that neutralize directly infected and highly infected cells, virulent fast viruses and cells) and memory lymphocytes for a faster response to a possible future challenge.
Immunity is the reaction of cells and tissues to foreign substances or pathogens, such as bacteria, viruses and parasites. It is distinguished as innate or natural immunity, and as adaptive or acquired immunity. Acquired immunity is distinguished as humoral immunity through the production of antibodies by plasma cells and as cellular immunity through T, B and immune-producing lymphocytes.
Spatio-temporal characteristics of the COVID-19 pandemic
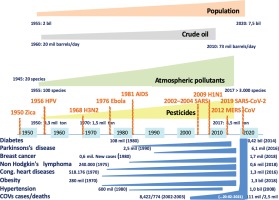
All lethal viruses have exogenous mechanisms of action related to their nature and are associated with endogenous mechanisms related to the immune system’s ability to respond to the existing human microbiome and food and energy status in combination with human, animal and environmental interactions. Anthony Fauci, the Director of the US National Institute of Allergy and Infectious Diseases, in a major article published 28 February 2020 in the New England Journal of Medicine, suggested that the COVID-19 mortality rate is ‘significantly less than 1%’. Older people over the age of 70 years with a weakened immune system have a 15–18% mortality rate, as in the 2009 H1N1 pandemic. According to CDC, in the COVID-19 pandemic, within a year, the cases were about 106.73 million and the death toll was about 2.33 million, i.e. 2.18% of the cases died or 0.031% of the world population, a mortality rate 10 times higher than that of the 2009 H1N1 pandemic, which had 1.6 million cases in one year and an average global mortality of 0.001–0.007%. Data from the CDC, WHO and the New England Journal of Medicine show that, compared to other viral pandemics, COVID-19 is also the first most prevalent pandemic in 219 countries, followed by the 2009 H1N1 viral pandemic, which spread to 214 countries. The history and spatio-temporal spread of pandemics in the context of globalization, the interaction of endogenous and exogenous factors in pathogenesis, clinical manifestation and prognosis of diseases show that there is a growing immune deficit (Figure 1).
Anthropogenic toxic agents and mechanisms of immune damage
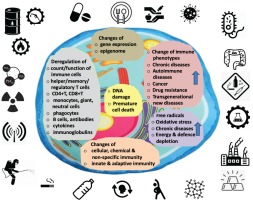
Today’s lifestyle has introduced various parameters that are not noticeable at first, but act chronically, causing an impact on the immune system later on. Such parameters can be chronic stress that indirectly deregulates the immune response through hormonal biological and neuroendocrine mechanisms, reducing the ability of cells to respond to anti-inflammatory signals and antibodies after antiviral vaccinations. Electric and magnetic fields also can interfere, and IARC researchers claim that the 5G technology is more powerful than the 4G, and in particular has been found to have detrimental effects on cell nucleotides, and therefore also on viruses. Occupational exposure to polychlorinated biphenyls (PCBs), PAHS, dioxins, benzene, and volatile organic compounds and crude oil derivatives have been shown to cause decreased antibody production and immunosuppression amongst others. Long-term exposure to organic solvents can disrupt the cellular immune response, increase antinuclear antibodies (ANA) and production of autoantibodies. Also, the long-term combination exposure to anthropogenic air pollutants (microparticles, ozone, volatile organic compounds, carbon monoxide, nitrogen etc.) have a strong combined effect on the immune response. The long-term exposure to lead, benzene, ethers, molybdenum and other octane enhancers in gasoline/mineral oils and halogenated dioxins, benzofurans, carbonates, and heavy metals, are carcinogens that can cause suppression of the immune cells and can be endocrine disruptors. Processed foods, reckless use of antibiotics in farm animals, pesticide use in crops, chemical food additives and the increased consumption of genetically modified foods, can have a cumulative and synergistic toxic effect on the immune system (Figure 2).
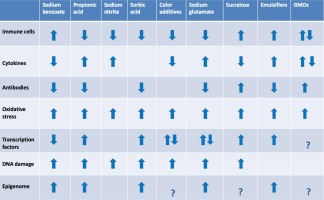
Figure 2
Immune disorders from long-term consumption of common chemical food additives and genetically modified foods
Perinatal exposure to heavy metals (cadmium, lead, arsenic, nickel, mercury, selenium etc.) can cause immune dysfunction and reprogramming of the immunophenotype. Smoking suppresses innate and adaptive immune responses, affects the number and function of immune cells, causes epigenetic changes in depth of many generations, and deregulates the expression of many transcription factors that control the expression of genes and enzymes of inflammation, autoimmunity and carcinogenesis. Ionizing radiation, even in small doses, substantially and persistently reshapes the innate and adaptive immune system. Exposure to phthalates, organochlorines, perfluorochemicals, polychlorinated biphenyls, dibenzofurans, dioxins, diphenols etc., mediated by oxidative, hormonal, biochemical, genotoxic, transcriptional and epigenetic mechanisms, negatively affects the innate and adaptive immune response leading to an increase in the immune deficit. Interactions between drug consumption and the immune system can alter the immune response, trigger resistance, alter the genome and microbiome, and the effectiveness of medications.
Collectively, the multifactorial effect of anthropogenic pollutants, xenobiotics and the achievements of modern technology on the immune response is illustrated in Figure 3.
Effects of chemical weapons and particulate matter on immune response and epidemic pandemic prevalence
In World War I, the majority of deaths were due to the Spanish Flu killing 50–100 million (3–5% global population) and infecting 500 million people, between 1918 and 1920. Some studies have focused on the susceptibility to the 1918 influenza pandemic due to ‘weakened immune system of the soldiers’1. CDC data on US life expectancy in 1918, influenza mortality by age, death rates in the USA by month and socioeconomic influenza impacts, enhanced the indications that soldiers exposed to mustard gas and other chemical agents in WWI played a key role in the 1918 flu onset, prevalence, global spread, and mortality due to their chemical immunosuppression2. The conjunction of soldiers, chemical gases, pigs, ducks, geese and horses at a large British Army camp in France during WWI, provided the growth conditions for the killer flu strain and the emergence of the ‘Spanish’ influenza pandemic of 1918–19193. Aerosol transmission of influenza requires up to 27000 times fewer virions to induce the equivalent disease4.
Similarly, some studies correlate atmospheric dispersion and transport of viral aerosols on the epidemiology of influenza5. All the HA and NA subtypes found in pandemic strains in 1918 (H1N1), 1957 (H2N2), 1968 (H3N2), and 2009 (H1N1) cause sporadic human infections or outbreaks without establishing human lineages6. This is an indication that sulfur mustard and other chemicals may induce antigenic drift over time as the virus replicates7.
This correlation is obvious in virulence, clinical outcome and mortality of COVID-19 patients8 who were previously exposed to sulfur mustard gases9. Recently, air pollution was found to promote significant health impacts with the aid of aerosols10 even for SARS-CoV-2. SARS-CoV-2 is a new threat11 from an old enemy12. These short-term and long-term health impacts of air pollution were found to be reduced during COVID-19 lockdowns in China and Europe13, indicating that particulate matter (PM2.5) is a potential SARS-CoV-2 carrier14.
The effect of lockdown on surface PM2.5 concentrations, the avoidance of premature deaths due to reduced PM2.5 concentrations and improvement of air quality during the lockdown period in China and Europe in 2020 indicate that there is a link between the SARS-CoV-2 RNA-laden particulate matter and the urban or enclosed polluted environment. In addition, exposure to particulate matter increases ACE2 expression in the lungs, which facilitates SARS-CoV-2 viral adhesion, indicating that particulate matter could be both a direct and indirect transmission model for SARS-CoV-2 infection15.
CONCLUSION
Xenobiotics, pollutants from anthropogenic activities, the negative effects of modern lifestyles and diets, radiation and the reckless use of new technologies are damaging the natural and acquired immunity, creating an immune deficit, increasing health costs, inefficiency and ineffectiveness of confronting vulnerability to infections, new and persistent multi-generational diseases and outbreaks of epidemics and pandemics, as in the case of COVID-19.
Many viruses, especially RNA viruses, such as the influenza virus and SARS-CoV-2 virus, develop unpredictable resistance to drugs and vaccines, even in a single short replication cycle. Chemical, pharmaceutical and environmental agents interfere with the resistance mechanisms and because of this intervention, the influenza virus and SARS-CoV-2 have a greater ability to bypass the immune system or make special drugs and vaccines unreliable.
It is no coincidence that in one year, COVID-19 became the first pandemic in number of cases and deaths in the last 100 years. COVID-19 has shown that this chronic lack of prevention and preparation can lead to unpredictable outbreaks with unexpected consequences. Therefore, in this time period, with this particular growth model and increasing morbidity, with a rapidly mutating SARS-CoV-2, it is obvious that controlling the COVID-19 pandemic is a difficult task.
Given the WHO finding that global health costs are now approaching $10 trillion, the annual growth rate of the pharmaceutical industry and rising morbidity prove that the modern growth model and its regulators prefer to pass on responsibilities for increased morbidity to individuals, and blaming the economic and social costs on the global population. When we consider that it took 30 years to fully prove that smoking causes cancer, that the use of lead in fuel was the biggest mistake of the 20th century, that nuclear testing had to stop, that atmospheric and organic persistent pollutants are pathogenic, then today during the COVID-19 pandemic, we do not have the luxury of past mistakes and cannot afford to wait as long.
The current bioassay model of chronic exposure is inadequate. Competent regulators evaluate just the toxicity of each chemical separately or harmful agent. Today, the synergistic and cumulative effect of the mixtures to which humans are daily exposed in real life conditions is not properly evaluated. The immunotoxic effects of xenobiotics can be evaluated by immunopathological, humoral, cellular and non-specific immunity parameters.
Modern toxicology along with other sciences such as chemistry, biology, genetics, technology and the environment, can give reliable, realistic and sustainable proposals for solutions.