INTRODUCTION
The International Labor Organization (ILO) considers work as a determinant of health and it defines workplace health promotion (WHP) as a proactive approach that involves collaborative efforts by employers, employees, and society to enhance the health and well-being of individuals at work1. This holistic strategy aims not only to prevent occupational injuries and illnesses, but also to improve the overall quality of life for workers. By integrating various health initiatives, such as safety protocols, wellness programs, and supportive work environments, WHP seeks to create a culture where health and well-being are prioritized. The ultimate goal is to contribute to a healthy, motivated, and productive workforce, which in turn can lead to increased organizational performance, decreased absenteeism, and economic benefits2.
The determinants of health within WHP encompass a wide range of factors that might influence employees’ physical, mental, and social well-being. They include work environment, lifestyle choices, social and community context, economic stability, access to health services and education3. A safe and supportive work environment, coupled with opportunities for healthy lifestyle choices can significantly impact workers’ health outcomes4.
Within the healthcare setting, the importance of prioritizing the health and safety of healthcare workers (HCWs) cannot be overstated. In fact, HCWs face unique occupational challenges that may negatively affect their health, including exposure to long and irregular working hours, high levels of stress, and potentially harmful environmental factors5-7. Among these challenges, night shift work (NSW) stands out as a particularly striking concern, due to its disruptive effects on circadian rhythms and sleep patterns, with several attributable short-term and long-term health consequences8. Exposure to light at night suppresses the production of melatonin, a hormone critical for regulating sleep-wake cycles and maintaining circadian rhythms9. This disruption can lead to immediate effects such as impaired alertness and cognitive performance, as well as long-term physiological changes10. Chronic circadian disruption has been linked to metabolic imbalances, including insulin resistance and obesity, increased inflammation, and alterations in lipid metabolism11. These changes collectively contribute to the heightened risks of cardiovascular diseases, metabolic disorders, and certain types of cancer, such as breast cancer in women12. Nurses, doctors, and other medical personnel frequently work night shifts to ensure round-the-clock patient care in hospitals and healthcare facilities, thereby being constantly exposed to high-impact occupational risks13.
Despite the abundance of WHP studies published, there is a need for programs tailored for healthcare personnel14,15. Addressing these gaps through novel research initiatives is crucial for developing effective WHP strategies resolving challenges specific of the HCWs. Such initiatives are essential not only for safeguarding HCWs’ health, but also for fostering a supportive work environment that promotes their overall well-being and longevity in their profession, finally identifying susceptible individuals16.
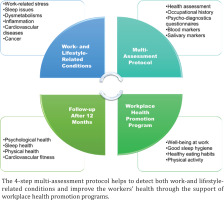
To this aim, this protocol proposes a comprehensive framework to assess the multifaceted health impacts of risks associated to work in healthcare sector, including NSW. This integrated assessment will utilize a variety of tools, including validated questionnaires to gauge HCWs’ overall fitness, work ability, sleep quality, daytime sleepiness, and dietary habits (i.e. Well-Being Questionnaire, Work Ability Index, Pittsburgh Sleep Quality Index, Epworth Sleepiness Scale, Adherence Score to Mediterranean Diet). Furthermore, blood and salivary biomarker analyses (circulating inflammatory cytokines, lipid profiles, vitamin D, salivary cortisol, alpha-amylase, and melatonin) will provide insights into several parameters such as: liver and renal functions, lipid profiles, inflammatory markers, sleep health, and stress levels. Following the assessment, the HCWs will receive suggestions and informative material to improve their lifestyle, and nutritional habits to support their well-being. Also, workers will be offered a follow-up visit at 12 months to verify the effectiveness of these interventions, ensuring that they are appropriately tailored to support their challenging work activities (Figure 1).
METHODS
Study design and participants
This study employs a prospective observational design to investigate the effects of NSW and other occupational risk linked with hospital work on the health and well-being of HCWs employed in a university hospital setting. NSW is defined as work carried out for at least 3 hours per daily shift (or a certain proportion of yearly working time) over a period of 7 hours, including the time from midnight to 5 a.m.17. The study population comprises HCWs who engage in NSW as part of their regular work schedule. The control population includes HCWs not engaged in NSW. Inclusion criteria for both groups are as follows: aged 20–65 years, having worked at least for six consecutive months in the hospital, and no previous medical history of cancer, including breast cancer.
Ethical considerations
Informed consent will be obtained from all participants prior to their participation to the study. This study has received approval from the Ethics Committee of the University Hospital ‘G. Martino’, Messina, Italy (C.E. protocol 40/19; 27 September 2019).
Study protocol
The protocol consists of three main components (described in detail below): 1) comprehensive medical and occupational assessment, 2) administration of validated self-assessment questionnaires and dietary tools, and 3) collection and analysis of biomarkers in blood and saliva samples.
Based on the outcomes of the assessment, HCWs will receive tailored health advice concerning well-being, sleep health, dietary habits, and cardiovascular health. This approach ensures that each HCW receives personalized recommendations to improve their overall health and mitigate the risks associated with NSW. Additionally, after 12 months, the same protocol will be applied to the enrolled workers, and comparisons between baseline and endpoint results will be performed. In detail, HCWs will be re-evaluated to assess the effectiveness of the WHP interventions implemented. This follow-up aims to verify whether the strategies designed to moderate the occupational risks have yielded positive outcomes.
Medical, occupational history and biometrical assessment
According to Italian legislation, HCWs are required to undergo a compulsory medical surveillance. This occupational health surveillance is overseen by a designated occupational physician and it includes a series of health evaluations aimed at monitoring and safeguarding the health and safety of HCWs, particularly in relation to their specific job functions and potential exposure to occupational hazards. The occupational physician conducts these evaluations at regular intervals, typically once a year. The evaluations consist of medical examinations, assessment of medical history, and various health screenings and tests, such as blood tests, vision tests, and lung function tests, to ensure that HCWs are fit to perform their duties and to identify any early signs of work-related health issues.
On that occasion, a multidisciplinary team, composed of occupational physicians and psychologists, will explain the aim of the investigation to the HCWs, perform the medical assessment, administer the validated questionnaires, and collect blood and salivary samples. The medical assessment includes a review of past medical conditions, medical and occupational exposure history, in particular regarding NSW schedules and duration, and several biometric measurements (Table 1). Subsequent to the baseline, these measurements will be repeated at the follow-up at 12 months.
Table 1
Summary of medical assessment protocol
Self-assessment questionnaires
In Table 2 are listed the panel of validated self-assessment tools administered to HCWs to assess three main aspects of their health and well-being: 1) occupational well-being, 2) sleep health, and 3) dietary health.
Table 2
Summary of self-assessment tools employed in the study protocol
| Aspect | Questionnaire | Description | Methods | Health advice |
|---|---|---|---|---|
| Occupational well-being | NIOSH Worker Well-Being Questionnaire (WellBQ)30 | Assesses job satisfaction, stress levels, work-life balance, and perceptions of workplace support. | 20 to 40 items covering various aspects of well-being. Identifies strengths and areas for improvement in the work environment. | Recommendations include stress management techniques, work-life balance strategies, and enhancements in workplace support systems. |
| Work Ability Index (WAI)5,31 | Evaluates work ability based on physical and mental capabilities, job demands, and health status. | 7 items related to current work ability, diagnosed illnesses, sick leave, and mental resources. | Interventions focus on improving physical and mental work ability, addressing health issues, and optimizing job demands. | |
| Sleep health | Pittsburgh Sleep Quality Index (PSQI)32,33 | Evaluates sleep quality over a one-month period, assessing factors like sleep duration, efficiency, and daytime dysfunction and identifies sleep disturbances. | 19 items grouped into 7 component scores. Higher scores indicate poorer sleep quality. | Advice on improving sleep hygiene, optimizing sleep environments, and managing shift schedules to enhance sleep quality. |
| Epworth Sleepiness Scale (ESS)34,35 | Measures daytime sleepiness by assessing the likelihood of dozing off in various situations. | 8 items, with higher scores indicating increased daytime sleepiness. | Recommendations include strategies to reduce daytime sleepiness and improve alertness, such as sleep hygiene practices and lifestyle adjustments. | |
| Dietary health | MEDI-lite questionnaire36 | Assesses adherence to the Mediterranean diet by evaluating the frequency of consumption of various food groups. | 9 items assessing daily consumption of fruit, vegetables, cereals, meat, dairy, alcohol, and olive oil, and weekly consumption of legumes and fish. | Nutritional guidance to promote balanced diets and improve adherence to dietary recommendations, emphasizing the Mediterranean diet principles. |
| Dietary diary | Records detailed dietary intake to assess nutrient intake and habits over a three-month period. | Participants maintain a detailed diary of all food and beverages consumed, including portion sizes and meal timing. Reviewed by healthcare professionals. | Feedback on dietary habits, recommendations for healthier food choices, portion control, and strategies to achieve specific dietary objectives. |
Collection of blood and salivary samples and analysis of biomarkers
Both at the baseline and at the follow-up at 12 months, blood and saliva samples are collected from participants for the analysis of several biomarkers associated with various physiological processes and health outcomes. Blood samples are collected during the medical surveillance visit, via venipuncture and stored appropriately according to standard laboratory protocols to maintain sample integrity and stability for subsequent analyses.
Saliva samples are collected via passive drool with a saliva collection aid (validated gold standard for saliva sampling) at two different timepoints: at 8 a.m. and at 10 p.m. (workers will be instructed on how to use the passive droll kit and store the sample). Both samples, upon collection, will be stored at -20°C until further processing (Table 3).
Table 3
Summary of blood and saliva tests
Calculation of the individual risk score
The individual risk score provides an accurate assessment, which takes into account: age, total serum cholesterol HDL and systolic blood pressure; anti-hypertensive therapy is also included in the assessment, taking into account that the systolic blood pressure level is influenced by specific drug effects. Anti-hypertensive therapy is also an indicator of longstanding hypertension. Finally, smocking habits have been taken into account18,19. Overall, according to the Italian Istituto Superiore di Sanità, to calculate total weight of risk factors, the following formula is used:
where E is age, C-T is total-cholesterol, C-HDL is HDL-cholesterol, PAS is artery systolic pressure, AIT is antihypertensive therapy, S is sex, and D is diabetes.
Finally, the Cardiovascular Risk Index (IRCV) may be obtained from: IRCV=100×(1-0.889-RF).
Statistical analyses
Quantitative data obtained from questionnaires and biomarker analyses are compiled and subjected to statistical analysis using appropriate methods, such as descriptive statistics, correlation analysis, and multivariate regression modeling. Statistical analyses will be adjusted for potential confounding variables to ensure the validity and reliability of the findings. Data processing and statistical analyses will be performed using IBM SPSS Statistics v23 for Windows (IBM Corp, Armonk, NY, USA) and GraphPad Prism version 9.0 for Windows (GraphPad Software, La Jolla, CA, USA). For all statistical analyses, differences will be considered significant with p<0.05 (*p<0.05; **p<0.01; ***p<0.001; and ****p<0.0001).
DISCUSSION
The workplace is a key setting for health promotion, given the possibility of reaching many people20. Employers can implement WHP programs to enhance employees’ health and job performance through interventions that raise awareness of actions to address many modifiable health risk factors21. However, research on WHP is limited, with no defined standard procedures in program definitions, activities, implementation, and outcomes22. Despite these challenges, several studies show positive effects of WHP on employee health and productivity, although the evidence in healthcare sector is still limited23. This study protocol aims to contribute to the evidence base for WHP among HCWs.
The key finding of this study protocol will be that a multidimensional perspective to assessing and improving the health of healthcare workers (HCWs) exposed to non-standard work schedules (NSW) can effectively address various health risks. The integration of subjective and objective data within this study protocol provides a comprehensive approach to understand the multifaceted impact of NSW and other occupational risks on HCWs. This holistic assessment encompasses three critical aspects: well-being, sleep health, and dietary habits, each evaluated through a combination of validated self-assessment questionnaires and biomarker analyses.
In detail, well-being is a crucial determinant of overall health and productivity in the workplace, especially in hospital settings24. The NIOSH WellBQ and the WAI questionnaires are employed to measure HCWs’ perceptions of job satisfaction, stress levels, work-life balance, and workplace support. These subjective reports are complemented by objective biomarker measurements, including circulating inflammatory markers (IL-1, IL-6), metabolic indicators and, also, salivary cortisol and alpha-amylase levels, may provide physiological insights into the impact of occupational stressors on short- and long-term health outcomes5. Additionally, increased susceptibility to cardiovascular diseases, can be assessed by correlating chronic inflammation markers, lipidemic and glycemic blood profiles, ECG and bioelectrical impedance measurements with persistent reports of poor well-being and work capacity7. Finally, the tailored calculation of IRCV may give direct information on the HCWs’ cardiovascular health.
Sleep health assessment focuses on evaluating HCWs’ sleep patterns, quality, and daytime sleepiness using tools such as the PSQI and the ESS. The integration of subjective sleep assessments with objective biomarkers enhances the reliability of findings, revealing the physiological consequences of sleep disturbances among HCWs. These include the measurement of salivary melatonin and cortisol levels, physiological indicators of circadian rhythm disruption and stress response, critical for understanding risks associated with night shift schedules that may compromise attention at work, impair cognitive function, and be correlated with possible long-term chronic diseases5.
Dietary health is evaluated through the MEDI-lite questionnaire, which assesses adherence to a Mediterranean diet, plus a detailed dietary diary that captures nutritional intake over time. Additionally, blood biomarkers such as lipid profiles and vitamin D levels offer objective measures of dietary impacts on both cardiovascular and metabolic health. This integrated approach not only identifies immediate dietary risks contributing to metabolic disorders but also underscores the long-term implications for chronic diseases like obesity, diabetes and stroke25. By linking self-reported dietary habits with objective biomarker data, the study elucidates the role of nutrition in mitigating or exacerbating health risks associated with NSW. In addition, the use of a dietary diary increases self-consciousness of diet behaviors, allowing the adoption of novel healthy habits26.
Overall, the integration of subjective perceptions with objective physiological data enhances the validity and depth of the protocol’s findings. By identifying modifiable risk factors and their impact on workers’ health, the protocol aims to develop targeted interventions that promote HCWs’ well-being and mitigate occupational health risks. Following the assessments, personalized health advisories will guide HCWs toward improving their modifiable lifestyle risk factors, potentially enhancing work performance and reducing work-injuries and absenteeism. This approach benefits employees, employers, and patients alike, creating a ‘win-win’ scenario for all stakeholders27.
The application of this study protocol may have significant implications for WHP strategies tailored to the healthcare sector. By highlighting specific challenges faced by HCWs, such as irregular shift patterns, high stress levels and sleep disruption, the study underscores the need for proactive interventions that address both individual and organizational factors. These interventions may include policy changes to optimize work schedules, promote healthier sleep hygiene practices, and support dietary improvements among HCWs. Furthermore, the longitudinal design of this study, with a follow-up visit programmed at 12 months, will provide valuable insights into the true effectiveness of WHP interventions implemented.
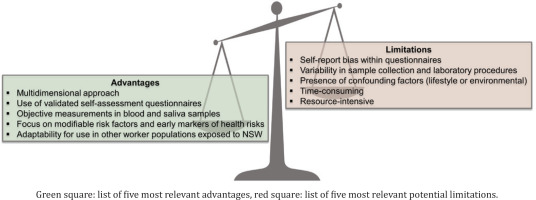
The developed protocol presents several advantages, such as collection of detailed information on how the various parameters assessed by blood and salivary biomarker analyses (e.g. circulating inflammatory cytokines, lipid profiles, vitamin D, salivary cortisol, alpha-amylase, and melatonin) are correlated with liver and kidney functions, lipid profiles, inflammatory markers, sleep health, and stress levels.
Additionally, it employs validated self-assessment questionnaires, ensuring reliable and consistent data collection from participants. Also, objective measurements in blood and saliva samples provide accurate and tangible health indicators. The focus on modifiable risk factors and early markers of health risks allows for proactive interventions, potentially mitigating long-term health issues. Moreover, the protocol’s adaptability for use in other worker populations exposed to non-standard work schedules (such as NSW) enhances its applicability and potential impact.
Limitations
However, the protocol also has limitations, including the risk of self-report bias within the questionnaires, which can affect the accuracy of the self-reported data. Moreover, variability in sample collection and laboratory procedures can introduce inconsistencies in the biological measurements. Also, the presence of confounding factors, such as lifestyle or environmental influences, may complicate the interpretation of results. Finally, the process might be time-consuming and resource-intensive, requiring significant investment in both time and materials to ensure comprehensive and accurate data collection and analysis. Advantages and limitations of the current study protocol are summarized in Figure 2.
Despite the possible challenges, this protocol focusses on the promotion of workers’ health by increasing the awareness regarding key modifiable risk factors, both work- and lifestyle-related, that might affect the health status and, in turn, the fitness to work. This approach is particularly relevant for HCWs, who often face long and irregular working hours, high stress levels, and exposure to potentially harmful environmental factors (chemical, physical, biological). By addressing these challenges, this protocol paves the way for novel and more standardized tailored interventions, crucial to effectively mitigate risks that are specific and heightened within the healthcare sector.
CONCLUSIONS
This study protocol not only advances our understanding of the health impacts of NSW among HCWs but also sets a precedent for comprehensive occupational health assessments in other industries. By integrating subjective perceptions with objective biomarker data, the protocol offers a robust framework for developing evidence-based interventions that prioritize the health and well-being of workers exposed to challenging occupational conditions, potentially identifying subjects with higher risks27. This approach holds the promise to inform policy decisions and practices aimed at enhancing workplace health and safety across diverse occupational settings, ultimately contributing to broader advancements in occupational medicine and public health28. Finally, the applicability of this protocol might extend beyond the healthcare sector, serving as a model for similar studies to be carried out in other worker populations exposed to NSW, such as those in transportation, manufacturing, hospitality, and emergency services29. By adapting this holistic approach to different occupational settings, the complex relationships between work-related factors, health behaviors, and disease outcomes can be further elucidated, contributing to the future standardization of WHP practices.